Diverticulitis
You have been diagnosed with Diverticulosis or Diverticulitis. This informational sheet will offer you some valuable information to help you understand your diagnosis. It offers suggestions for healthy living which will prevent progression of the disease.
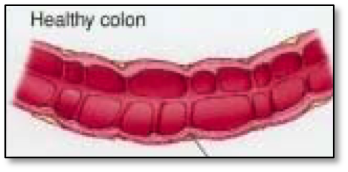
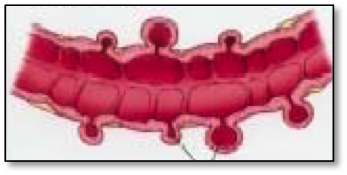
What are Diverticula?
Diverticula are little “pouches” of intestine. They form when the inner lining of the intestine pushes through the outer lining of the intestine. Nearly 20% of people over the age of 40 will have some diverticula. By the age of 70, nearly 70% of people will have diverticula of the colon. Only 15% of individuals who have diverticula develop any problems associated with their presence.
Why do diverticula form?
Pressures inside the colon cause the pouches to form. We know that diets low in fiber lead to constipation and higher pressures in the colon. If you have eaten a diet low in fiber all through your lifetime, you may be at higher risk of developing diverticula. People who suffer from other bowel disorders, such as irritable bowel syndrome, may also be at higher risk of forming diverticula.
What is Diverticulosis? How would I know that I had it?
Diverticulosis is the term used when a person is known to have diverticula of the colon. A person who has diverticulosis often will not know that they have it; in general, there are no symptoms. Some people, however, may complain of constipation, diarrhea, or tenderness in the area that is affected. Diverticulosis is often found when a person goes to have their colonoscopy at age 50 or 60.
What is Diverticulitis? How will I know if I have it?
Once you have been diagnosed with diverticulosis, you are at risk for developing diverticulitis. Diverticulitis is the swelling of diverticula that occurs when the pouches become blocked with contents of the intestine (usually pieces of undigested foods such as corn kernels, seeds, nuts, or indigestible fibers). A person with diverticulitis will have pain or tenderness (usually in the left lower area of the belly). The pain is intense and the person will often seek medical attention to alleviate the pain. A low grade fever, as well as an elevated white blood cell count may occur during a “flare up” of diverticulitis. “Flare ups” require medical attention, so if you have been diagnosed previously with diverticulosis, and you are having belly pain, you may now have developed “full blown” diverticulitis. Seek medical care as soon as possible.
Diverticulitis “Flare Ups” Require Prompt Medical Attention
The swelling and inflammation that occurs around inflamed diverticula can lead to a breakage of the pouch. This leads to bleeding and leakage of intestinal contents and germs into the body, which can lead to severe complications including death. If it is suspected (during physical examination) that you have a perforation of the intestine, a CT scan will be ordered to evaluate this. Bladder symptoms (painful urination, frequent urination, and a need to urinate “immediately”) may also occur if the area of involvement is close to nerves leading to the bladder. Be sure to report any urinary symptoms to your provider, as this may help aid in a proper diagnosis.
Treatment during “flare ups” of diverticulitis:
Bedrest is prescribed. You will NOT be prescribed pain medication. Avoid pain medicine including Tylenol. You should follow a liquid diet until you no longer have abdominal pain and fever. Special considerations will be made if you are diabetic.
Liquid Diet – Follow as long as you are having pain, constipation, or fever.
Juices Clear Apple Juice, White Grape Juice - NO PULP! Snacks Clear Jell-O (not sugar free). Popsicles without fruit or pulp. - NO PULP! Broth Clear chicken or beef broth Drinks Gatorade, Poweraid (not sugar free) - AVOID Caffeine, NO Energy Drinks Tea Avoid Caffeinated teas
If you do not improve or tolerate a fluid diet, you will be sent to the emergency room or hospital. During flare ups, antibiotics will be prescribed. Tell your provider if you are allergic to sulfa drugs. You will be given 2 separate antibiotics, and you should take both of them. If you continue to have fever or pain while using the antibiotics, be sure to call the provider and let them know if you are not feeling better. Always keep your follow up appointments during a flare up. Evaluation of your recovery is just as important as initial treatment.
What can I do to prevent serious problems?
As you can see, diverticulitis is a severe and complicated disease. Lifestyle Management has been very effective in reducing the progression of the disease in other people. Your adherence to a similar plan will greatly benefit your health.
Helpful tips of what to watch for:
DO THIS AVOID THIS
- Increase the fiber in your diet by regularly eating: Fruits Vegetables - especially root vegetables - Raw carrots Bran in its many forms Metamucil supplement
- 20 minutes of exercise daily In particular, aerobic exercise shown to help - Walk, run, jog, bike, Stairmaster
- Get plenty of fluids to avoid constipation
- Eat 5-6 small meals daily instead of 3 larger meals
Avoid foods with seeds or indigestible materials:
Corn, Popcorn
Seeds – all sources – watch for hidden seeds such as:
Strawberries (seeds on the outside), Okra seeds, Cucumber seeds, Tomato seeds, Fig seeds, Nut Hulls (peanut hulls, pecans, walnuts, almond hulls)
If you have had frequent “flare ups” of diverticulitis, if you have had complications during a past flare, or if you can not adhere to the above preventive plan of care, a different diet may be suggested, known as a “low residue diet.” However, “low residue” diets do lack certain nutritional benefits, and should only be used if the above diet has not been successful in keeping your disease under control. Ask your provider for more information on a “low residue” diet if your diverticulitis has not been well controlled.
Is there anything else I need to know?
Be sure to ask your provider questions regarding your diagnosis if there is anything that you do not understand. Your health depends on a good understanding and self management plan. Good health, not “good luck!”